NEONATAL CARE
By Andrea Nagel
Early next year,
the doors to the
new neonatal intensive care unit
(NICU) will open for the first time,
ready to start treating newborns with
increased needs for intensive care.
Because this is a new program, neo-
natal medical director Kathleen
Webb, M.D., hand-picked individuals
to create a neonatal stabilization team
(or NeST) that will respond to
cardiorespiratory emergencies
involving newborns up to 1 month
of age.
“It’s been a multiyear process to
make sure everyone is ready,” said
Cassy Oddy, birthing center charge
nurse. “Not only did we need to
develop the team and the tools, but
then we trained our current employ-
ees and each new hire. We hold
special training sessions and
simulations to keep everyone up to
speed.”
Although the NeST team is
helping to prep for the transi-
Building a NeST
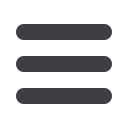
Rob Skinner, Cassy Oddy and Kristie Hiiva practice
neonatal resuscitation on a simulation mannequin.
T H E N E O N ATA L T E A M AT K O O T E N A I H E A LT H
I S W O R K I N G H A R D T O P R E PA R E F O R T H E N E W N I C U
tion, most of their work involves
preparing staff in the skills needed
to stabilize any emergency in the
delivery room. The core team that
developed the program consists
of Cassy as well as Dr. Webb,
Kristie Hiiva, neonatal intensive
care nurse; Rob Skinner, respira-
tory therapist; and Althea Davis,
clinical educator. Together, they
met for over six months outside of
work hours to develop the protocol,
tools and simulations needed to
train staff.
“They’ve taken the idea I pre-
sented to them and run with it.
I relate them to a NASCAR pit
crew,” Dr. Webb explained. “Every-
one jumps into position as soon as
they’re needed. It’s like a dance;
everyone has a role, place and
knows exactly what everyone else
is doing at any given point. When
you’re working to save an infant’s
life, every second matters.”
Although they frequently refer-
ence themselves as the NeST
team, Rob explained that
the term is for anyone that
received special training; is
serving in the roles of neo-
natal intensive care nurse,
labor and delivery charge
nurse, and respiratory thera-
pist; and is scheduled to be
part of the response team
for a particular shift. No
matter where the emer-
gency takes place throughout the
hospital, this team will respond.
“There’s nothing else like this
here,” Rob said. “This is the first
time we’ve had a multidisciplinary
team work together to develop a
program. We’re hoping this model
will spill over into other depart-
ments. It’s a unique opportunity
to partner and collaborate with
others—it has increased our
teamwork, communication and
respect we have for each other as
professionals.”
Dr. Webb’s core NeST team
travels throughout northern Idaho
to help prepare rural hospital staff
to resuscitate infants. They also
partnered with the Idaho Simula-
tion Network and JoDee Anderson,
M.D., from the Oregon Health
and Science University to provide
simulation-based neonatal resus-
citation training. This allows the
team to stay in Coeur d’Alene and
watch a live feed of another team’s
simulation scenario. They can then
offer suggestions to help improve
the quality of care for newborns
and premature babies throughout
our region.
“I see this team that’s improving
care and processes across medical
disciplines and the region, and I
admire them,” said Dr. Webb. “Of
all the things I’ve done at Kootenai
Health, this is what I’m most proud
of.”
B E S T F O R M O M A N D B A B Y
You can learn more about neonatal services at
Kootenai Health by visiting
KH.org/neonatology .Are you currently looking for an OB-GYN? Contact
Kootenai Clinic OB-GYN at
(208) 625-4970
.
8

















